PATTERNS AND INDICATIONS OF INTENSIVE CARE UNIT ADMISSIONS IN PATIENTS WITH NEUROLOGICAL AND NEUROSURGICAL CONDITIONS: A 5-YEAR RETROSPECTIVE ANALYSIS
DOI:
https://doi.org/10.5281/acs.v11i1.238Keywords:
ICU admission, neurocritical care, stroke, traumatic brain injury, outcomesAbstract
Background: Neurological and neurosurgical patients frequently require intensive care due to the risk of rapid deterioration. Understanding intensive care unit (ICU) admission patterns in this population is critical for planning and optimizing resource utilization. Our objective is to analyse demographic patterns, indications, and outcomes of ICU admissions among neurological and neurosurgical patients over a five-year period.
Methodology: A retrospective review of ICU admissions at the Lagos State University Teaching Hospital (LASUTH) between October 2019 and October 2024 was conducted. Data included demographics, primary diagnosis, indication for admission, length of stay, need for mechanical ventilation or vasopressors, and outcomes.
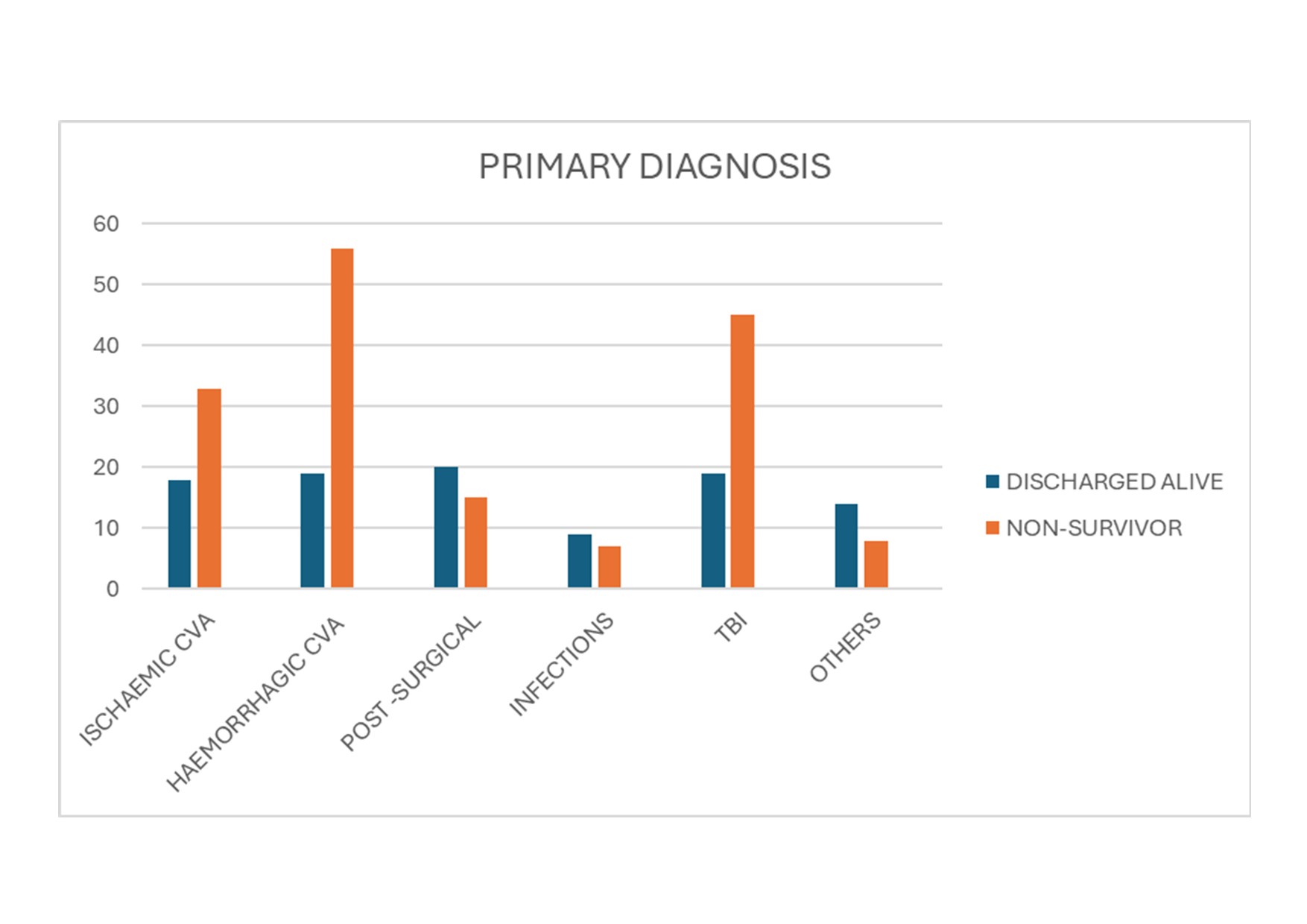
Results: Of the 1,118 ICU admissions over the study period, 263 (23.5%) were neurological/neurosurgical. Mean age was predominantly in the working-age group (18–60 years). Haemorrhagic cerebrovascular accident (CVA) (n=75, 28.524%) was the leading diagnosis, followed by traumatic brain injury (TBI) (n=64, 24.3%) and ischaemic CVA (n=51, 19.39%). The major indication for ICU admission was reduced consciousness requiring airway protection (76.4%). Mechanical ventilation was required in 88% and vasopressor support in 70%. Mortality was 38.40% (101 deaths), while 61.6% were discharged alive, with survival favouring younger patients.
Conclusion: CVA is the predominant reason for neuro-ICU admission. Mortality remains high, especially in older patients. Improved early referral systems, stroke awareness, and enhanced neurocritical care capacity are urgently needed in resource-limited settings.